Arrhythmias or disorders of heart rhythm are a group of diseases characterized by abnormality of heart beat. Our heart is expected to beat in a certain way. In an adult individual the heart normally beats 60 t0 100 times per minute, in a regular manner (that means a nearly constant interval between two beats ). There are some normal variations, like in children the heart beat is faster, in some healthy persons and trained athelets the heart beat can be slower, during sleep the heart beat is normally slower.
Definition of Arrhythmia:
Arrhythmia is defined as any deviation from this normal pattern of heart beat.
What are the types of Arrhythmia?
Heart rhythm disorders are basically of two types. When the Heart rate is abnormally high it is called TACHYCARDIA. When the heart rate is abnormally slow it is called BRADYCARDIA. There can be irregular heart beats even if the heart rate is between 60-100, those cases are also Arrhythmic.
What is the relation of arrhythmias to other heart diseases?
Arrhythmias can be divided into two types based on heart diseases
- Arrhythmias occurring in persons having no underlying structural heart disease are called- IDIOPATHIC ARRHYTHIMAS
- Arrhythmia also arise in persons who have underlying structural heart diseases.
What are the symptoms of Arrhythmia?
Arrhythmias due to slow heart rate (Bradycardia) commonly cause
- Lethargy
- Fatigue
- Palpitation
- Light headedness
- Syncope (Transient loss of consciousness followed by full recovery)
- Sudden death
Arrhythmias due to fast heart rate (Tachycardia) commonly produce symptoms of
- Palpitation
- Faintness and light headedness
- Syncope (Transient loss of consciousness followed by full recovery)
- Sudden death
- Reduced pumping capacity of heart and related symptoms
- Some arrhythmias like atrial fibrillation can produce abnormal clotting of blood inside heart which can migrate to brain to cause stroke and paralysis.
How serious are Arrhythmias?
Some arrhythmias are benign and non life threatening, but they cause troublesome symptoms of palpitation and skipped beats.
Some arrhythmias are life threatening and can cause even sudden death. It all depends on the origin and type of arrhythmias and any other underlying heart disease.
How to diagnose arrhythmia?
Arrhythmias are commonly diagnosed by
- ECG
- Holter monitoring
- Sometimes long term monitoring like – event recorders, loop recorders etc.
- In some case Cardiac Electrophysiological study is required to diagnose a rhythm disorder.
What are the treatments available?
- Some transient arrhythmias terminate on their own and don’t need any specific therapy
- Underlying cause needs to be treated like- drugs, electrolyte disturbances, etc
- Medicines are usually the first line treatment
- Catheter Ablation: It is a procedure done in cardiac cathlab where an arrhythmia is ablated commonly by application of radiofrequency energy inside the heart. It is a safe procedure with prospect for complete cure of the arrhythmia.
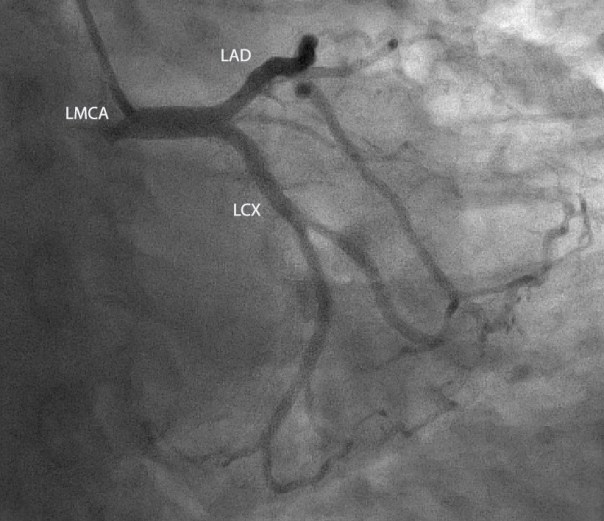
Left main coronary artery, left anterior descending and left circumflex coronary artery
Myocardial Infarction- Third Universal definition and classification
Definition of myocardial infarction
Criteria for acute myocardial infarction :
The term acute myocardial infarction (MI) should be used when there is evidence of myocardial necrosis in a clinical setting consistent with acute myocardial ischaemia. Under these conditions any one of the following criteria meets the diagnosis for MI:
• Detection of a rise and/or fall of cardiac biomarker values [preferably cardiac troponin (cTn)] with at least one value above the 99th percentile upper reference limit (URL) and with at least one of the following:
- Symptoms of ischaemia.
- New or presumed new significant ST-segment–T wave (ST–T) changes or new left bundle branch block (LBBB).
- Development of pathological Q waves in the ECG.
- Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality.
- Identification of an intracoronary thrombus by angiography or autopsy.
• Cardiac death with symptoms suggestive of myocardial ischaemia and presumed new ischaemic ECG changes or new LBBB, but death occurred before cardiac biomarkers were obtained,or before cardiac biomarker values would be increased.
• Percutaneous coronary intervention (PCI) related MI is arbitrarily defined by elevation of cTn values (>5 x 99th percentile URL) in patients with normal baseline values (≤99th percentileURL) or a rise of cTnvalues >20% if the baseline values are elevated and are stable or falling. Inaddition,either(i)symptoms suggestiveof myocardialischaemia or (ii) new ischaemic ECG changes or (iii) angiographicfindings consistent with a proceduralcomplication or (iv) imaging demonstration of new loss of viable myocardium or new regional wall motion abnormality are required.
• Stent thrombosis associated with MI when detected by coronary angiography or autopsy in the setting of myocardial ischaemia and with a rise and/or fall of cardiac biomarker values with at least one value above the 99th percentile URL.
• Coronary artery bypass grafting (CABG) related MI is arbitrarily defined by elevation of cardiac biomarker values (>10 x 99th percentile URL) in patients with normal baseline cTn values (≤99th percentile URL). In addition, either (i) new pathological Q waves or new LBBB,or (ii) angiographic documented new graft or new native coronary artery occlusion, or (iii) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality.
Criteria for prior myocardial infarction
Any one of the following criteria meets the diagnosis for prior MI:
• Pathological Q waves with or without symptoms in the absence of non-ischaemic causes. • Imaging evidence of a region of loss of viable myocardium that is thinned and fails to contract,in the absence of a non-ischaemic cause.
• Pathological findings of a prior MI
UNIVERSAL CLASSIFICATION OF MYOCARDIAL INFARCTION
Type 1: Spontaneous myocardial infarction
Spontaneous myocardial infarction related to atherosclerotic plaque rupture, ulceration, fissuring, erosion, or dissection with resulting intraluminal thrombus in one or more of the coronary arteries leading to decreased myocardial blood flow or distal platelet emboli with ensuing myocyte necrosis. The patient may have underlying severe CAD but on occasion non-obstructive or no CAD.
Type 2: Myocardial infarction secondary to an ischaemic imbalance
In instances of myocardial injury with necrosis where a condition other than CAD contributes to an imbalance between myocardial oxygen supply and/or demand, e.g.coronary endothelial dysfunction, coronary artery spasm, coronary embolism, tachy-/brady-arrhythmias, anaemia, respiratory failure, hypotension, and hypertension with or without LVH.
Type 3: Myocardial infarction resulting in death when biomarker values are unavailable
Cardiac death with symptoms suggestive of myocardial ischaemia and presumed new ischaemic ECG changes or new LBBB, but death occurring before blood samples could be obtained, before cardiac biomarker could rise, or in rare cases cardiac biomarkers were not collected.
Type 4a: Myocardial infarction related to percutaneous coronary intervention (PCI)
Myocardial infarction associated with PCI is arbitrarily defined by elevation of cTn values >5 x 99th percentile URL in patients with normal baseline values (£99th percentile URL) or a rise of cTn values >20% if the baseline values are elevated and are stable or falling. In addition, either (i) symptoms suggestive of myocardial chaemia, or (ii) new ischaemic ECG changes or new LBBB, or (iii) angiographic loss of patency of a major coronary artery or a side branch or persistent slow- or no-flow or embolization, or (iv) imaging demonstration of new loss of viable myocardium or new regional wall motion abnormality are required.
Type 4b: Myocardial infarction related to stent thrombosis
Myocardial infarction associated with stent thrombosis is detected by coronary angiography or autopsy in the setting of myocardial ischaemia and with a rise and/ or fall of cardiac biomarkers values with at least one value above the 99th percentile URL.
Type 5: Myocardial infarction related to coronary artery bypass grafting (CABG)
Myocardial infarction associated with CABG is arbitrarily defined by elevation of cardiac biomarker values >10 x 99th percentile URL in patients with normal baseline cTn values (£99th percentile URL).In addition,either (i) new pathological Q waves or new LBBB, or (ii) angiographic documented new graft or new native coronary artery occlusion, or (iii) imaging evidence of new loss of viable myocardium or new regional wall motion abnormality
Coronary artery disease
Coronary artery disease
The heart like any other organ in the body needs constant supply of blood to survive. Blood reaches different parts of the heart through the coronary arteries. Coronary arteries are of vital importance for the sustenance of life.
The different normal functions of the coronary arteries include:
1. Carrying blood to different parts of the heart
2. Regulating blood supply to the heart in the face of varying blood pressure
3. Increasing blood supply to the heart in the face of increased cardiac demand like during exercise.
The coronary arterial system: Can be divided into four parts
1. Left main coronary artery (LMCA)
Which divides into
2. Left anterior descending artery (LAD) And
3. Left circumflex artery (LCX)
4. Right coronary artery (RCA)
What is coronary artery disease (CAD)
Any disease which involves coronary arteries is CAD. Usually the most common form is reduction in the size of the coronary arteries. Many disease conditions can result in coronary artery disease but the most common cause of CAD is atherosclerosis. Other diseases like autoimmune diseases, congenital diseases can result in CAD.
Why CAD occurs?
CAD occurs due to a variety of reasons, which are called risk factors. You can read more about risk factors here.
What are the types of CAD?
CAD is a septum of diseases and it is divided to two categories
1. Chronic stable angina (CSA): In CSA there is a pattern of chest discomfort associated with exertion or emotional excitability. The occurrence of angina is after a predictable amount of work.
2. Acute coronary syndromes ( ACS)
ACS are are again divided into three types
A. Unstable angina: When there is new onset angina, worsening of previous angina, rest angina, it is called unstable angina
B. Non-ST elevation myocardial infarction
C. ST elevation myocardial infarction – the classic heart attack
This classification is important for the point of view of management and the aggressiveness of treatment.
What are the symptoms of coronary artery disease?
A. Angina : Chest pain or discomfort .
B. Angina equivalents – fatigue , dyspnoea (shortness of breath) , eructations, palpitation
C. Sudden onset acute severe chest pain
D. Cold sweating
Read more about symptoms of heart disease here.
What to do?
First of all see your doctor for evaluation and treatment. Some of the general management modalities are discussed here.
Investigations
For the diagnosis of CAD the following investigations may be needed:
A. ECG – is of central importance in CAD. ECG in many occasions shows changes suggestive of reduced myocardial blood flow
B. Stress test – Different types of stress tests are available like treadmill test, nuclear stress tests. A stress test can be done by performing exercise on a treadmill or by giving drugs in patients who are unable to do exercise. It is done when the symptoms are not typical and ECG changes are not typical.
C. Echocardiography – is for assessment of structure and function of heart
D. CT coronary angiography – It is a noninvasive imaging modality for the diagnosis of CAD. It is like any other CT scan. Contrast injections are given to visualize the coronary arteries
E. MRI coronary angiography – Not very widely used for imaging of coronary arteries
F. Coronary angiography – this is the gold standard for the diagnosis of coronary artery disease and any percutaneous treatment for CAD can be done in the same setting
Treatment:
A. Risk factor control – Risk factor control is one of the most effective interventions for reducing the impact of coronary heart disease. Proper control of blood pressure, diabetes, quitting smoking, treatment of abnormalities of cholesterol are some of the steps that greatly reduce the incidence and prevalence of CAD.
B. Medications- Patients with CAD will on some medications indefinitely (usually life long). For chronic stable angina, the first line of treatment is usually medical management. Even patients who undergo coronary artery stenting or bypass surgery need to take medicines life long.
C. Coronary angiography and percutaneous coronary interventions are usually advised for patients who have more serious symptoms or for whom symptoms are not easily controlled with medicines. In presence of certain high risk factors patients should undergo early angiography and intervention or surgery
D. Coronary artery bypass grafting (CABG)
Drugs used in treatment of CAD:
1. Anti- platelets e.g. Aspirin, Clopidogrel, Prasugrel, ticagrelor, etc
2. Statins e.g. rosuvastatin, atorvastatin etc
C. Beta blockers (metoprolol, bisoprolol etc)
D. Ace inhibitors or angiotensin receptor blockers
E. Anticoagulants (heparin)
F. Nitrates
G. Nikorandil
H. Ranolazine
I. Trimetazadine
H. Therapies for refractory angina
Details about each class of drug I will post each week( Monday )
So please follow up
Cardiac interventions for CAD:
Known as percutaneous coronary intervention(PCI). In this procedure coronary angiography is done and then stenting is done as required.
Coronary artery bypass grafting:
CABG may be needed where PCI is not feasible or doesn’t give optimum results.
Finally there are a spectrum of patients who have drug refractory angina who are not suitable for PCI or CABG. They have refractory angina and the treatment options are limited in such patients.
Conclusion: Coronary artery disease is the leading cause of death and suffering in the world. The most common symptoms include chest pain, shortness of breath. It is diagnosed by ECG, stress tests, coronary angiography etc. The treatment include risk factor reduction, medical management and PCI or bypass surgery as needed.
Key words: Patient information, Coronary artery disease, heart disease, coronary angiography, ECG, Angina, CAD, PCI, CABG
Right coronary artery

Heart Disease in Women
Heart Disease in Women
This topic will cover important and unique issues related to cardiovascular diseases in women. I will simplify it as much as I can. The problem of women’s heart is complex. Feed-backs or follow-up comments are welcome.
Is Heart disease really important for females?
The answer is YES ABSOLUTELY. Diseases of the heart are the leading causes of death and suffering in women. Every 1 in 3 female deaths is caused by heart disease. This amounts to more deaths from heart disease than from stroke, lung cancer and breast cancer combined. About half of these deaths (1 in 6) are caused by coronary artery disease (coronary artery = arteries supplying blood to heart muscles). A 40 years old female has a life time risk of development of cardiovascular disease of about 32%. The life time risk of heart failure is more in females than males, every 1 in 6 women is at risk of developing heart failure, whereas every 1 in 9 males is at risk of developing heart failure. Now I hope the problem of cardiovascular diseases in women is well understood. There is a need to be vigilant about your heart.
Heart disease in women:
Risk factors are the conditions or diseases which increase the chances of having heart disease (you can read more about risk factors under patient information page). The major risk factors of having coronary artery disease in females are same as in males. They are:
- Hypertension
- Diabetes mellitus
- High blood cholesterol
- Smoking
- Obesity
- Family history of coronary artery disease.
There are important differences in the manner in which these risk factors are tackled in women as compared to men.
Hypertension is 15% more common in females than males. Diabetes mellitus is as common in females as in males if not higher. Similarly elevated blood cholesterol in females is as common as in males. Obesity is more common in females than males. The things which are unique to women are that
- They are less likely to receive adequate treatment for these risk factors
- Guideline recommended treatment is used to a lesser extent in females
- Females are more likely to discontinue treatment
- They adopt life style modifications like regular walking, less often.
All these factors make females uniquely susceptible to coronary artery disease.
It has been seen that even after a heart attack there is delay in seeking medical attention. The response to treatment of heart attack is also less favourable in females.
In conclusion, the idea of writing this article is to create an awareness that women are equally or sometimes more prone for cardiovascular disease than men. They experience less symptoms which leads to delay in seeking medical attention. Even after medical consultation they are more likely to be undertreated and less likely to comply with medications. So it is high time that medical professionals and patients take notice of these facts and act accordingly
What to do ?
The following measures help to reduce the morbidity and mortality of cardiovascular diseases in women
1. Regular checking of blood sugar for diabetes
2. Regular checking for BP
3. Life style modification like – regular physical exercise, weight control, low salt intake
4. Consult your doctor for any symptoms
5. Regular intake of medicines
Thank you
Dr. S. N. Panda
